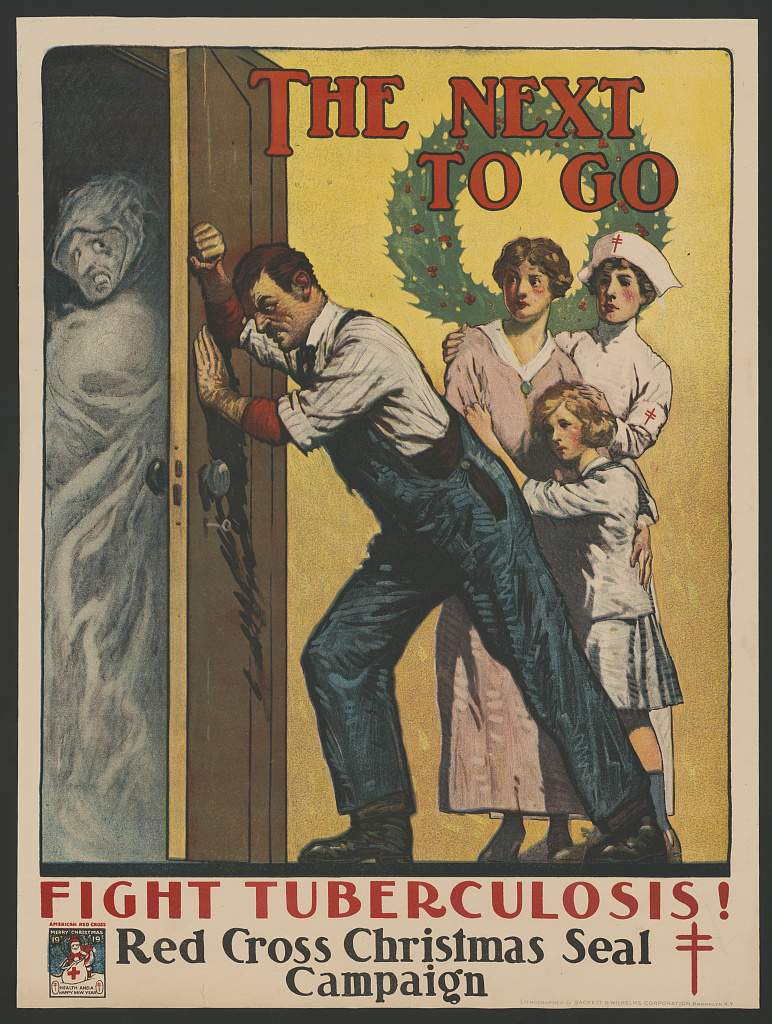
Red Cross Poster, 1919 – Fight Tuberculosis!
Just another nerd.
The New England Vampire Panic is apparently a bit of a misnomer–media reporting of the panic used the term “vampire” but the folks in New England caught up in the panic did not.
Still, up until the late 19th century there apparently persisted a folk belief that tuberculosis was caused by TB sufferers draining the life from their family members, including after death.
The [tuberculosis] infection spreads easily among a family; thus, when one family member died of consumption, other members were often infected and gradually lost their health. People believed that this was due to the deceased TB sufferer draining the life from other family members. The belief that consumption was spread in this way was widely held in New England and in Europe.
In an attempt to protect the survivors and ward off the effects of consumption, bodies of those who had died of the disease were exhumed and examined. The corpse was deemed to be feeding on the living if it was determined to be unusually fresh, especially if the heart or other organs contained liquid blood. After the culprit was identified, there were a number of proposed ways to stop the attacks. The most benign of these was simply to turn the body over in its grave. In other cases, families would burn the “fresh” organs and rebury the body; occasionally, the body would be decapitated. Affected family members would also inhale smoke from the burned organs or consume the ashes in a further attempt to cure the consumption.
Fascinating documentary from American Experience on tuberculosis in the United States which as the title notes is believed to be the deadliest disease in human history, and thanks to drug resistant strains was declared a global health emergency by the World Health Organization in 1993.
https://www.youtube.com/watch?v=gsaBmJjIDpM
Is smoking a major contributing factor to high incidence of tuberculosis in the developing world? A study of tuberculosis sufferers in India suggests that it is.
The BBC reports that researchers at the Epidemiological Research Center in Madras, India, calculated that as many as half of the tuberculosis deaths among men in that country would not have occurred if it were not for smoking, and that as many as 75 percent of tuberculosis cases in the country can be traced directly to smoking.
Tuberculosis can apparently lie dormant and inactive in the lungs, but smoking reduces the lung’s natural defenses against tuberculosis.
The researchers compared 43,000 men who died in the late 1990s with 35,000 men who were still living. Of the 43,000 deaths, 4,000 were from tuberculosis and researchers estimated that only about 2,000 of those would have occurred if it hadn’t been for smoking.
The BBC quoted Indian researcher Vendhan Gajalakshmi as saying,
Almost 200,000 people a year in India die from TB because they smoked — and half of these are still only in their 30s, 40s or early 50s when they die. Our study indicates that in rural India about 12% of smokers, but only 3% of non-smokers, die prematurely from TB.
Sources:
Smoking and mortality from tuberculosis and other diseases in India: retrospective study of 43000 adult male deaths and 35000 controls.
Vendhan Gajalakshmi, Richard Petob, Thanjavur Santhanakrishna Kanakaa and Prabhat Jhac, The Lancet, Vol. 362, Issue 9383, 16 August 2003, Pages 507-515.
Smoking feeds India TB scourge. The BBC, August 15, 2003.
Study links men’s smoking, tuberculosis deaths in India. Associated Press, August 15, 2003.
The World Health Organization recently released a report on the state of tuberculosis in the world and called on donor nations to provide funds to distribute and monitor the administration of anti-tuberculosis drugs in the developing world.
The WHO’s basic conclusion is that the tuberculosis situation is declining fueled by the twin killers of AIDS and poverty. WHO estimates that one in three of the world’s 42 million HIV positive individuals also has tuberculosis.
Back in the early 1990s WHO declared tuberculosis to be a global emergency, and the situation with the disease today is much worse.
The cost of drugs that combat tuberculosis is only $10 for a complete regimen of drugs that will cure about 95 percent of cases. But in order for this to work, the entire series of drugs must be taken on a timetable. Poor health care systems in the developing world mean that even among individuals who receive drugs, few actually complete the entire regimen. This not only renders the drugs useless, but also dramatically increases the risks of more drug-resistant strains of tuberculosis.
According to WHO estimates, fewer than 1 in 3 African patients receives the entire series of drugs, and in Russia that percentage is even lower.
Aside from the devastating toll the disease takes among those afflicted with it, there is a bigger danger that a drug resistant form of the disease could emerge that would spread the disease along the lines of India. India is the epicenter of the tuberculosis epidemic with two million new cases annually.
WHO estimates that it needs another $4 billion or so to fulfill its plan to stop the spread of tuberculosis by 2005.
Sources:
WHO calls for widespread free access to anti-TB drugs for people living with HIV. Press Release, World Health Organization, July 15, 2003.
TB drugs ‘should be free’. The BBC, July 15, 2003.
TB advocacy report 2003. World Health Organization, 2003.
A report by the World Health Organization, UNICEF and the World Bank concluded that 3 out of 4 children around the world now have access to essential vaccines. But, of course, that means that fully 25 percent of the world’s children are not routinely vaccinated against childhood diseases.
According to The State of the World’s Vaccines and Immunization, as many as 37 million children under the age of one are not immunized against the six major vaccine-preventable diseases of childhood: tuberculosis, tetanus, whooping cough, diphtheria, polio and measles.
Moreover, the inability of underdeveloped countries to pay for vaccines combined with ongoing property rights disputes over ownership of drugs and vaccines in such countries acts as disincentive for further research into vaccines for diseases that plague the developing world.
According to the report,
Today, vaccine manufacturers have little commercial incentive to develop vaccines against diseases such as HIV/AIDS, TB and malaria, which kill millions of people in developing countries, but relatively few in the developed world. For example, of the approximately US$600 million a year invested in HIV vaccine research, the majority comes from the US National Institutes of Health (a public sector institution). To put that amount in perspective, in 1999, research spending on drugs to treat HIV/AIDS was about US$3 billion in Europe and the United States alone. Other diseases fare just as badly. In the 1996 report Investing in Health Research and Development, WHO highlighted some of the distortions in global health research funding. At the time of the study, acute respiratory infections, diarrheal disease and TB — which together account for almost 8 million deaths a year, mainly among the poor — attracted an estimated US$99-133 million. . . By contrast, more was spent on research into asthma — an estimated US $127-158 million — which accounts for 218,000 deaths a year worldwide.
Of course the report ignores the possibility that the relatively heavy funding in asthma is what is responsible for such a low worldwide death toll, but even so the amount estimated to be spent on research into diseases that kill 8 million people is staggeringly low.
Source:
Vaccine policy leaves millions at risk. The BBC, November 20, 2002.
State of the World’s Vaccines and Immunization Report (PDF). UNICEF, 2002.