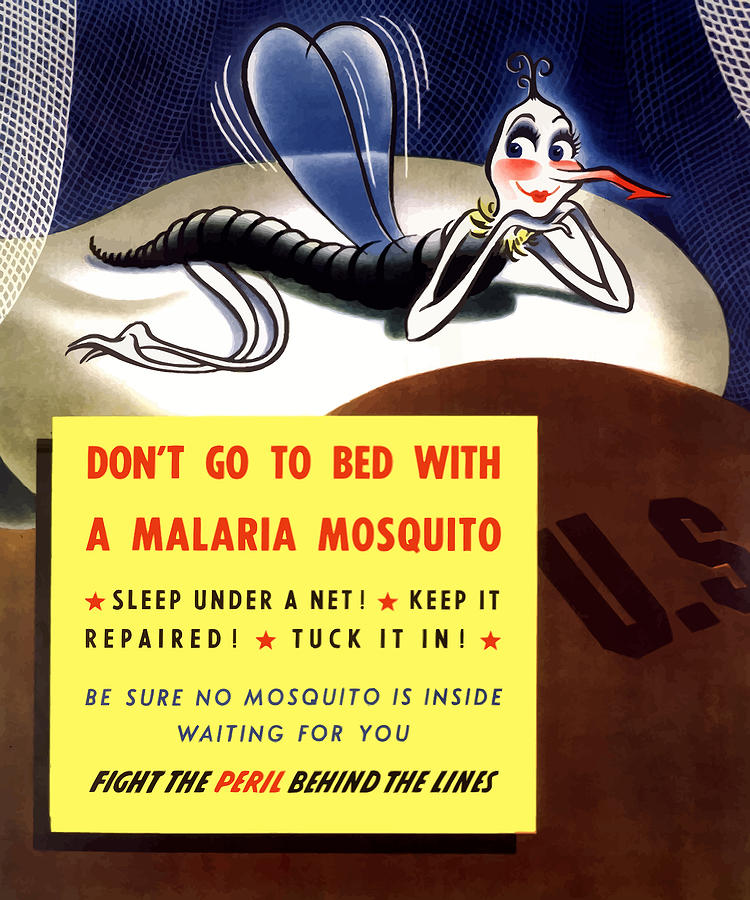
World War II Propaganda Poster–Don’t Go To Bed With A Malaria Mosquito
Just another nerd.
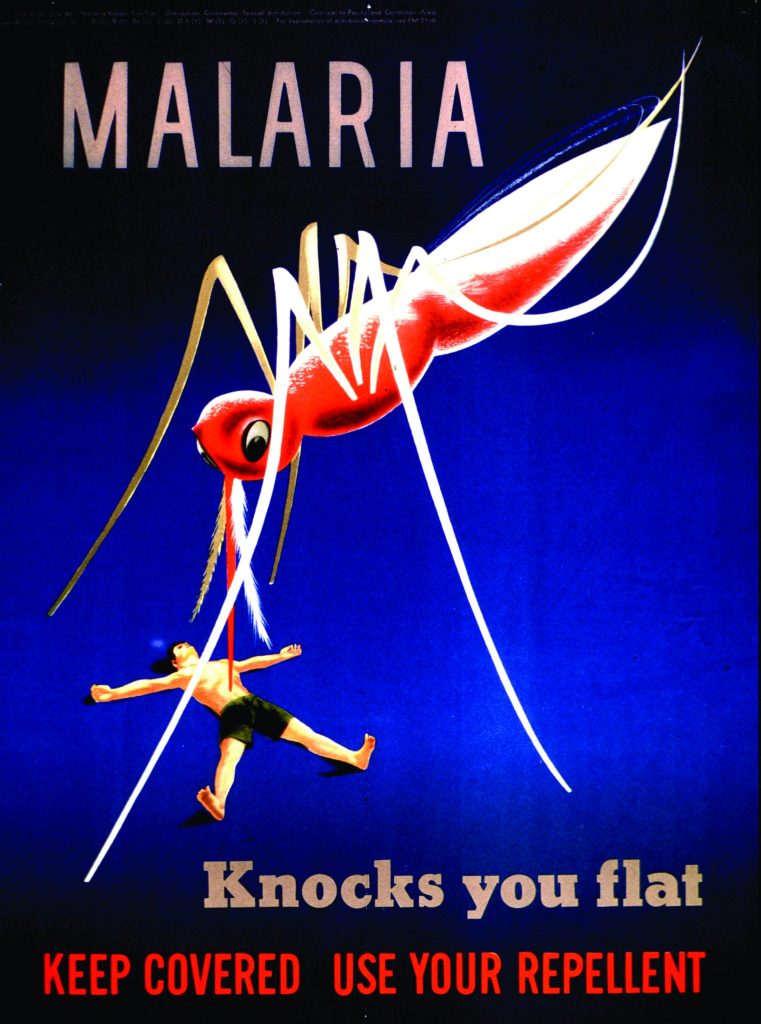
Malaria was a significant problem for the United States war effort in the Pacific Theater of Operations.

In September, Nature Biotechnology published a paper by researchers describing their efforts to use CRISPR-Cas9 in a laboratory setting to prevent reproduction in a population of mosquitoes that transmit malaria to human beings,
In the human malaria vector Anopheles gambiae, the gene doublesex (Agdsx) encodes two alternatively spliced transcripts, dsx-female (AgdsxF) and dsx-male (AgdsxM), that control differentiation of the two sexes. The female transcript, unlike the male, contains an exon (exon 5) whose sequence is highly conserved in all Anopheles mosquitoes so far analyzed. We found that CRISPR–Cas9-targeted disruption of the intron 4–exon 5 boundary aimed at blocking the formation of functional AgdsxF did not affect male development or fertility, whereas females homozygous for the disrupted allele showed an intersex phenotype and complete sterility. A CRISPR–Cas9 gene drive construct targeting this same sequence spread rapidly in caged mosquitoes, reaching 100% prevalence within 7–11 generations while progressively reducing egg production to the point of total population collapse. Owing to functional constraint of the target sequence, no selection of alleles resistant to the gene drive occurred in these laboratory experiments. Cas9-resistant variants arose in each generation at the target site but did not block the spread of the drive
Researchers at the Howard Hughes Medical Institute have discovered how malaria parasites evade the human immune system on their way to infecting people. Their discovery was published in Nature in late 2005.
Essentially, the parasite has a number of cloaking mechanisms, and keeps most of them in reserve. As it encounters resistance from the human immune system the parasite is capable of tailoring its cloaking to the immune system. The parasite has dozens of genes designed to get past the immune system, and what the researchers found was that as one gene was activated, that also trigger the suppression of the others. In this way, the malaria parasite is able to try one method after another to infect the host, and reduce the risk that the host might quickly develop an immunity against most or all of the parasite’s cloaking methods.
As HHMI researcher Alan Cowman put it in a press release announcing the discovery,
It’s like a leopard being able to change its spots. New forms come up, and the immune system beats them down again. Because of this a lot of people think you need five years of constant exposure to malaria in its different disguises to gain immunity.
Unfortunately too many people, especially children, die long before they can develop immunities to the malaria parasite’s numerous tricks. Even among people who develop immunity, that immunity can be quickly lost if the individual is not consistently exposed to malaria parasites.
This sort of research could one day lead to a treatment for malaria that might, for example, defeat this mechanism and allow for those exposed to malaria to quickly develop immune responses to all of its cloaking mechanisms.
Sources:
How malaria dupes immune system. BBC, December 29, 2005.
Scientists Lift Malaria’s Cloak of Invisibility. Press Release, Howard Hughes Medical Institute, December 28, 2005.
An Indian malaria researcher recently reported on the success of initial pilot projects to use fish that eat mosquito larvae to control malaria.
This is a traditional method that was commonly used before the introduction of DDT in the 1950s and is once again being looked at as part of the solution to malaria.
The idea is to stock ponds, rivers and wells with fish like guppies that feed on the mosquito larvae. Dr. VP Sharma of the COuncil for Medical Research said that while the technique could not be used everywhere, in places where it was appropriate to use it had virtually eliminated a subspecies of malaria-carrying mosquito in some districts where mosquito-eating fish were introduced.
According to the BBC, Sharma credited the fish introduction program for India’s falling malaria rate which declined by about 200,000 cases per year after the program’s introduction. Sharma did add that, “It will take another five years before the real impact would be known” from the numerous fish introduction programs that the World Bank is underwriting.
Source:
Fish eat away at malaria in India. Richard Black, BBC, January 5, 2004.